The Truth About Sciatica: What Actually Causes It and What Treatments Work Best
Sciatica is one of the most misunderstood conditions in spine care. Most people believe it is a diagnosis, when in reality, sciatica is a symptom, a warning sign that something is irritating or compressing the sciatic nerve.
If you are experiencing pain that travels from your lower back into your hip, buttock, or down your leg, understanding what is truly ausing your sciatica is the key to choosing the right treatment and avoiding chronic problems.
At The Center for Total Back Care in Mesa, we specialize in finding the root cause of sciatica, not just masking the pain.
What Is Sciatica Really?
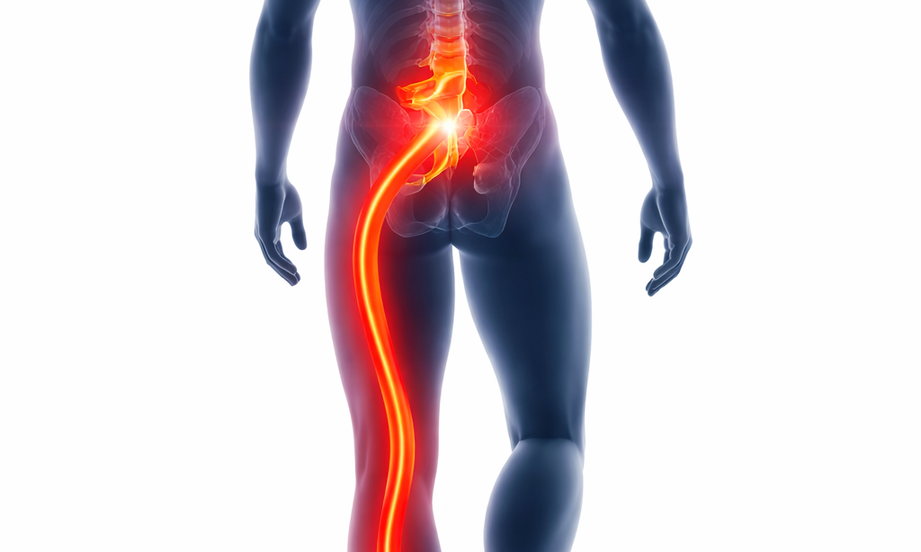
Sciatica refers to nerve pain caused by irritation or compression of the sciatic nerve, which is the largest nerve in the body. This nerve originates in the lower lumbar spine, travels through the pelvis and buttocks, and runs down each leg.
Sciatic pain can include:
- Sharp or burning pain down one leg.
- Numbness or tingling in the leg or foot.
- Weakness in the affected leg.
- Pain with sitting, bending, or lifting.
It is important to understand, sciatica is not a muscle problem, and it is rarely caused by “tight hamstrings” or simple inflammation alone.
What Actually Causes Sciatica?
1. Lumbar Disc Herniation or Bulge (Most Common Cause)
The most frequent cause of sciatica is a disc bulge or herniation in the lumbar spine, typically at L4-L5 or L5-S1.
When a disc bulges or herniates:
- It often triggers inflammation which can irritate the nerve.
- Pain can often be referred along the path of the sciatic nerve.
- It can press directly on a spinal nerve root.
This type of sciatica often causes leg pain that is worse than back pain and may worsen with sitting or forward bending.
2. Piriformis Syndrome: A Less Common but Real Cause of Sciatic Pain
While most true sciatica originates in the lumbar spine, piriformis syndrome is another condition that can mimic sciatic nerve pain and is often misunderstood.
The piriformis is a small, deep muscle found in the buttock region. While in most people (around 80-90%) the sciatic nerve passes below the piriformis muscle. With anatomical variations which occur in about 10-20% of the population, the sciatic nerve either pierces through the muscle or passes above it. When this muscle becomes tight, inflamed, or dysfunctional, it can irritate the sciatic nerve.
Key Features of Piriformis Syndrome
Piriformis-related sciatic pain often presents differently than disc-related sciatica:
- Pain typically begins in the buttock rather than the lower back.
- Leg pain may worsen with prolonged sitting, driving, or crossing the legs.
- Symptoms often improve with walking or changing positions.
- Neurological reflex changes or muscle weakness are usually absent.
Importantly, piriformis syndrome does not involve disc compression or spinal instability, which is why imaging studies such as MRI are often normal in these cases.
Why Piriformis Syndrome Is Often Misdiagnosed
Piriformis syndrome is often over diagnosed when spinal causes are missed, assumed when imaging does not show a large disc herniation or treated without confirming whether the spine is truly stable.
In clinical practice, true piriformis syndrome is far less common than disc-related sciatica, but it does exist and must be ruled in or out.
This is why exact assessment matters. Treating piriformis syndrome when the real issue is spinal disc pressure can delay recovery and prolong symptoms.
How Piriformis Syndrome Is Treated
When piriformis syndrome found, treatment may include:
- Targeted soft tissue work, such as dry needling
- Specific stretching and movement retraining
- Addressing pelvic and hip mechanics
- Correcting contributing posture or activity patterns
Unlike disc-related sciatica, spinal decompression is not usually indicated for piriformis syndrome.
3. Spinal Instability and Weak Supporting Muscles
Most patients are surprised to learn that muscle weakness—not tightness—is a major contributor to chronic sciatica.
Deep spinal stabilizers such as the multifidus muscles play a critical role in protecting discs and nerves. When these muscles are weak or inhibited:
- The spine becomes unstable.
- Discs are overloaded.
- Nerve compression is more likely to persist.
This is why passive treatments alone often fail.
4. Degenerative Disc Changes (Is Usually Not the Pain Source)
Disc degeneration is common, especially with age. However:
- Degeneration alone does not usually cause pain.
- Problems occur when degeneration leads to instability which can result in disc involvement which may cause irritation to the nerve root or nerve compression.
Imaging findings must be correlated with objective findings, including strength testing and clinical symptoms, not treated in isolation.
5. Spinal Stenosis or Arthritic Changes
In some cases, narrowing of the spinal canal or nerve openings can compress the sciatic nerve roots, especially with standing or walking. This is more common in older adults and often presents differently than disc-related sciatica.
Why Proper Diagnosis Is Critical
Sciatic pain can feel similar regardless of the cause, but the treatment approach must match the underlying problem.
At The Center for Total Back Care in Mesa, we differentiate between:
- Disc-related nerve compression.
- Spinal instability and weakness
- Less common causes such as piriformis syndrome
Using clinical evaluation, objective spinal strength testing and movement assessment, we can determine the root cause of the nerve irritation, not just where it hurts.
Why Many Sciatica Treatments Fail
Most sciatica treatments focus on temporary symptom relief, not correction of the underlying problem.
Common limitations include:
- Pain medications that mask symptoms
- Injections that reduce inflammation temporarily
- Generic exercise programs that do not stabilize the spine.
Without addressing disc pressure and spinal weakness, sciatica often returns.
What Treatments Actually Work Best for Sciatica?
1. Accurate Diagnosis Comes First
Effective treatment starts with identifying:
- Whether the cause is disc-related, instability-related, or both.
- Which spinal levels are involved.
- If the piriformis is contributing to the pain.
- Whether muscles are weak or neurologically inhibited.
At our Mesa clinic, we use MedX medical spinal strength testing to objectively measure lumbar and cervical strength. This allows us to pinpoint a hidden weakness that MRIs cannot show.
2. Non-Surgical Spinal Decompression (VAX-D)
For disc-related sciatica, VAX-D spinal decompression can:
- Reduce pressure inside the disc.
- Improve disc hydration.
- Relieve nerve compression without surgery.
VAX-D non surgical spinal decompression is not appropriate in every case, but when used correctly, it is highly effective.
3. Targeted Spinal Rehabilitation (Not Generic Exercise)
True recovery requires specific strengthening of the deep spinal stabilizers, especially the multifidus.
MedX rehabilitation:
- Isolates spinal muscles safely.
- Provides measurable progress.
- Restores long-term stability.
This approach is vastly different from general core exercises or home programs.
4. Chiropractic Care and Supportive Therapies
Chiropractic adjustments, when combined with:
- Spinal rehab
- Decompression
- Soft tissue therapies including dry needling.
It can help restore motion, reduce nerve irritation, and improve outcomes. Adjustments alone are rarely sufficient for chronic sciatica.
Can Sciatica Be Prevented From Coming Back?
Yes, if the underlying cause is corrected.
Patients who only treat pain often experience repeated flare-ups. Patients who:
- Restore spinal strength.
- Reduce disc stress.
- Improve movement mechanics.
Have significantly better long-term results.
When Should You Seek Help?
You should seek evaluation if:
- Sciatic pain lasts more than a few days, or you have had more than one episode.
- Pain is worsening or traveling further down the leg.
- You experience numbness, tingling, or weakness.
- When previous treatments have failed.
Early intervention will not only help minimize problems in the future but can often prevent chronic nerve damage.
Sciatica Treatment in Mesa, AZ
If you are dealing with sciatica and want answers, not guesswork, our team at The Center for Total Back Care specializes in evidence-based, non-surgical solutions for disc and nerve-related pain.
We serve patients throughout Mesa, Chandler, Gilbert, and Tempe, with a focus on long-term results.
Schedule your comprehensive evaluation today at: totalback.com